What is gingivitis in cats
When the cats' gums are red, swollen, and sometimes bled, we talk of gingivitis. It is crucial to determine the cause of it for two reasons. On the one hand, different treatment methods depend on the cause; conversely, gingivitis and possible secondary diseases can quickly become chronic and challenging to treat.
The vet should make an accurate history of the cat's diseases because depending on the symptoms and history, knowledge of all this can be helpful to rule out possible viral infections. A radiographic examination with dental x-rays is essential in suspected FORL (feline odontoclastic resorptive lesions). If tartar is present, it should be removed by the vet under general anesthesia.
Which cats are most at risk?
Any cat is susceptible to oral cavity disease. However, some cats are at greater risk than others, starting with older, immunocompromised animals (such as those infected with FIV) and calicivirus carriers. In addition, cats that go out a lot are likely to come across many carriers and are more likely to get infected.
What causes gingivitis in cats
Gums inflammation can be caused by the presence of foreign bodies in the animal's mouth (for example, blades of grass). But the cause could also be periodontium (periodontitis) inflammation or other organ diseases (like kidney failure). However, infectious diseases – caused by bacteria or viruses - are the most common causes of gingivitis in cats.
It can be very diverse and, for this reason, the diagnosis is solely up to the veterinarian. The doctor will examine the animal's mouth and, if necessary, may prescribe an X-ray to check the condition of the dental roots. Last but not least, some lab tests, such as blood tests, may be required to check for any previous conditions that may have fueled the disorder.
Cats gingivitis symptoms
Cats are true experts at hiding their pain. In nature, they are not allowed to show weakness and are therefore experts at covering their ailments. It's when the pain escalates that we humans realize something is wrong with our favorite animal.
Gingivitis becomes evident through typical signs of inflammation such as redness and swelling. In addition, a reddened gum line often forms around the teeth, but if you can't look into your cat's mouth, know that gingivitis can also manifest through the behavior.
You may also often notice unpleasant halitosis. For example, animals that suffer from mouth pain salivate very often, and in this case, cats drool, or they keep their heads tilted when eating, an apparent state of distress.
Since the pain becomes present and persistent, cats try to get rid of it, scratching the mouth with their paw. Very often, even eating becomes torture; cats affected by the disease may start to eat and then run away while eating.
While cuddling, you may also notice that your cat suffers from halitosis or makes sounds with the lower jaw when yawning.
The case of feline chronic gingivostomatitis
It is a specific disease of cats. Several viruses (calicivirus, FIV, FeLV, feline herpes virus) can cause chronic feline gingivostomatitis. The cat's immune response is no longer adapted, and the entire oral cavity is infected. It is challenging to treat and can be identified by various symptoms: pain, permanent gum line, lack of appetite and weight loss, dirty coat (the cat no longer washes), halitosis, excessive salivation.
How to treat gingivitis in cats
Currently, there are several ways to treat cat gingivitis:
Pain relief treatment - anti-inflammatory drugs (non-steroid) should be used, ideally combined with opioids if the animal requires them. Corticosteroids can sometimes be used for refractory cases and for those whose teeth cannot be extracted. Immunomodulators can be used instead of steroids to manage excessive inflammatory reactions, but the financial impact of this choice is high.
Use of antibiotics - their use is not automatic since it only limits the risk of the appearance or recurrence of a bacterial infection in the case of hygienic measures that are not respected or challenging to apply.
Dental surgery – when the damage proves to be more critical than expected, tartar removal is usually coupled with dental extractions. Some studies, particularly in cats, have demonstrated the effectiveness of a total extraction of teeth without visible signs of discomfort to feed afterward. It avoids residual pain or lesions not detected during a simple tartar removal. It is better to eat without teeth (digestion does not start in the mouth as it does in humans) than to have pain that is not always visible to the owner, preventing the cat from getting better.
This treatment can be differentiated based on gingivitis etiology in cats:
Calicivirus gingivitis - there is no specific treatment. However, antibiotics may be administered to prevent bacterial infections that have occurred.
Retrovirus gingivitis - antibiotics can be administered. However, if no clinical improvement is seen, corticosteroids can be used to reduce inflammation. In addition, immunotherapy has recently begun to be used, which consists of administering interferon-alpha and Propionibacterium acnes to act as immunostimulants to reduce immunodepression.
Lymphoplasmacytic gingivitis - antibiotic therapy is used, although it does not give striking results. Corticosteroids are also valuable for reducing inflammation and dental hygiene as a maintenance treatment.
How to prevent gingivitis in cats
Unfortunately, it is tough to prevent the presence of foreign bodies or tumors in cats. However, hygiene measures and vaccinations can protect cats against gingivitis. According to the guidelines for the immunization of small animals of the Standing Committee on Vaccination for Veterinary Medicine, a first step could be to get them a vaccination against:
Feline herpesvirus (FHV-1), feline calicivirus (FCV), and feline parvovirus (FPV). Vaccination occurs at 8, 12, and 16 weeks of age and after 15 months of age and revaccination may be recommended by the manufacturer every 1 to 3 years;
Non-systematic vaccination against feline leukemia virus (FeLV), e.g., in free-ranging cats after a negative test result: from 8 weeks of age at intervals of about one month and a final injection after one year.
Simple steps can reduce the risk of developing the disease:
Prefer solid food – Solid food helps to prevent tartar from building up a mechanical action (friction) that a soft food will not have. Most of the notable cat food brands offer kibbles whose composition is enriched with "anti-tartar" ingredients. There are also kibbles specially designed for oral hygiene maintenance (shape, composition...). However, be careful: an animal that eats too quickly and does not chew its food will not benefit from the expected mechanical effect.
Give him something to chew - at least once or twice a week, you can offer something to chew or a hard nylon toy. Be careful that these don't break or splinter, which your pet could swallow. Check that these toys are pet toys and the instructions for use.
Brush your cat's teeth - plaque begins to redeposit eight hours after tartar removal. Therefore, two to three times a week, you can brush your cat's teeth with toothpaste and a soft (preferably pet) toothbrush. If your cat seems to consider brushing his teeth torture, you can use anti-tartar supplements instead of teeth brushing. In this case, choose odorless and unflavored supplements mixed into drinking water or food and change the taste.
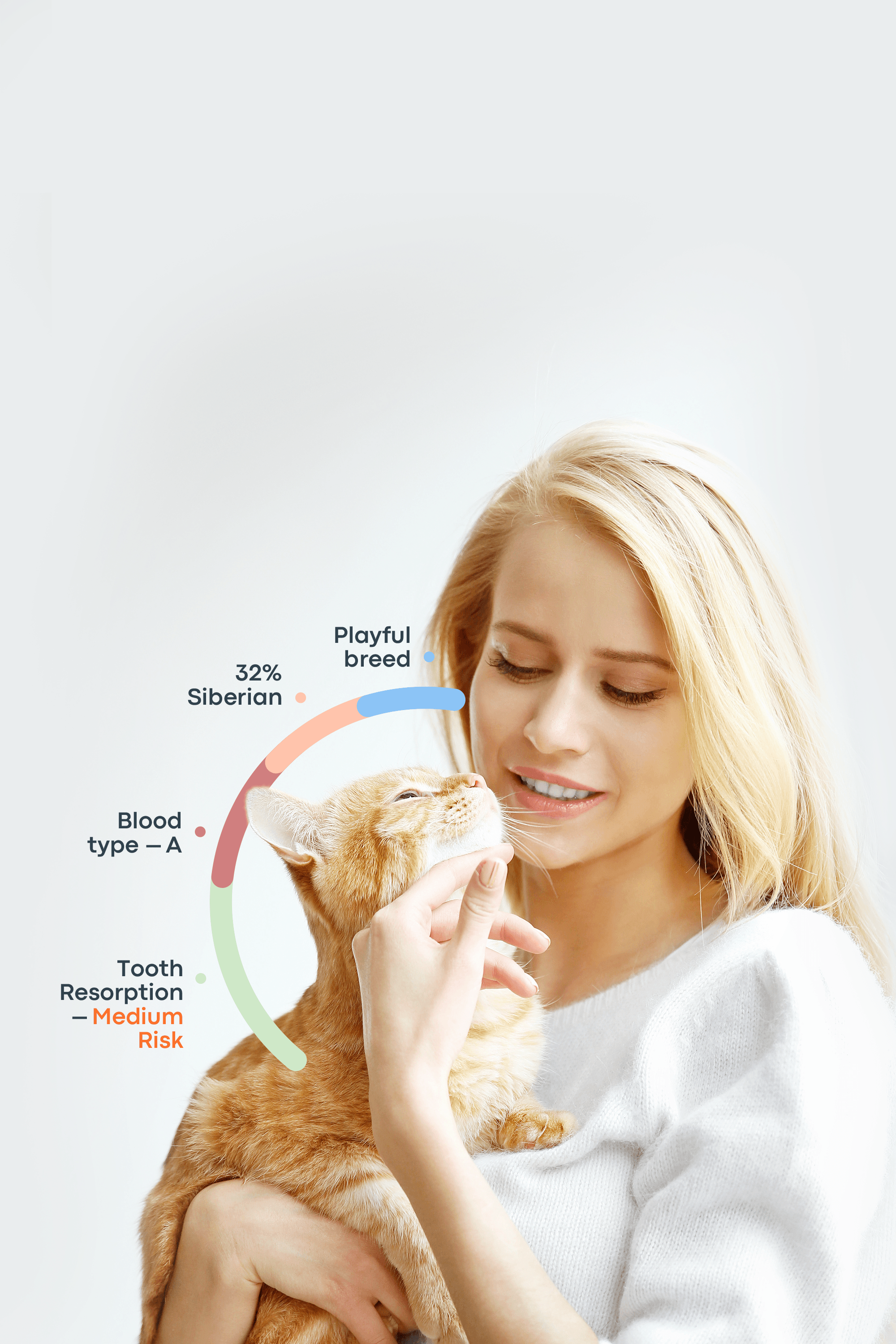
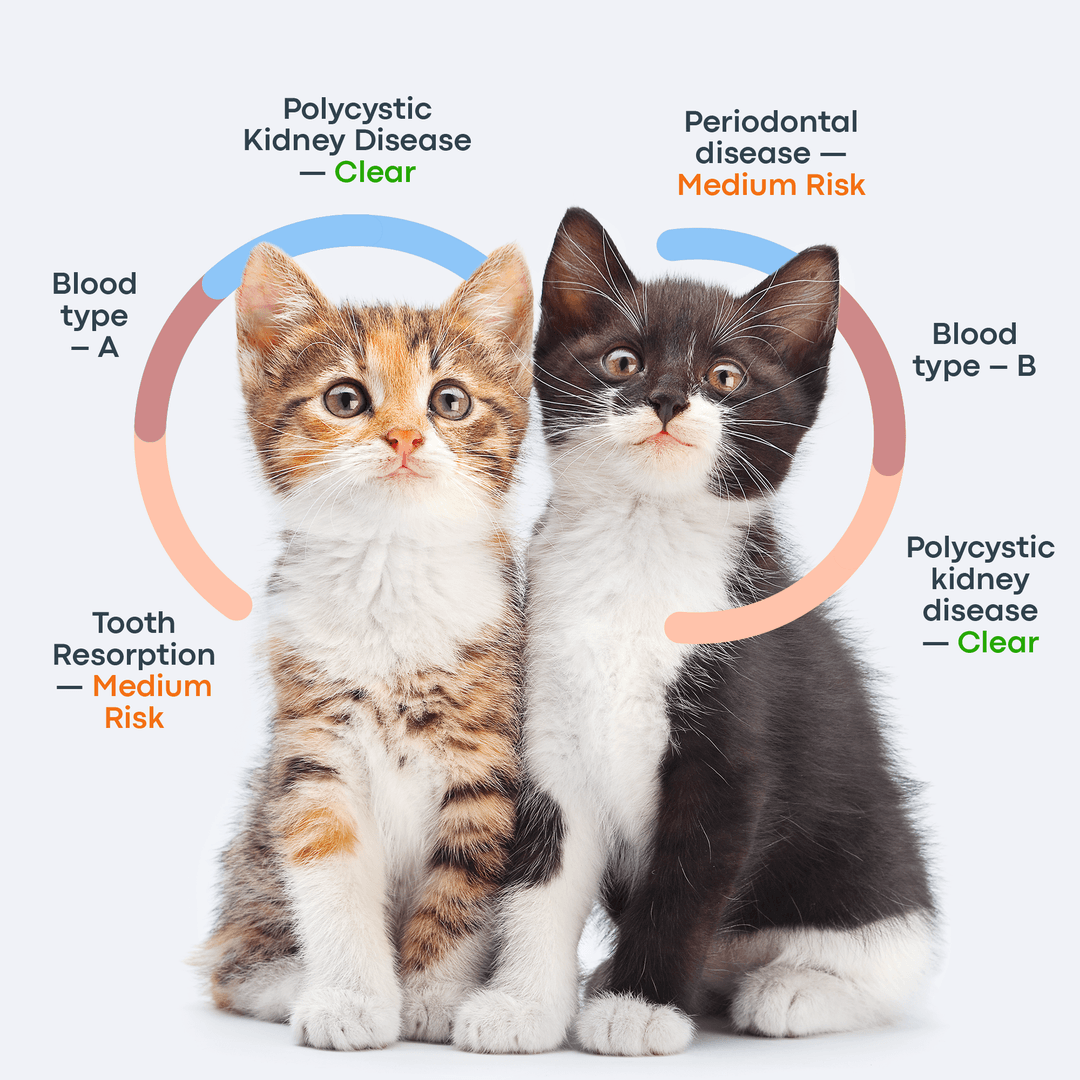
Cat gingivitis profoundly affects your cat's quality of life. By following these oral hygiene guidelines, you can help keep your cat healthy and comfortable. Instead, if you want to know your cat’s dental health, you can use this test.